Pure Grit
Stories of Remarkable People Living with Physical Disabilty
“A must read”
—Julie Dussliere, Chief of Paralympic Sport, U.S. Olympic & Paralympic Committee
“Each of the nineteen stories is superb in its own right, and as a collection this book is a joy to read.”
—Rachel Byrne, Executive Director, Cerebral Palsy Foundation, New York
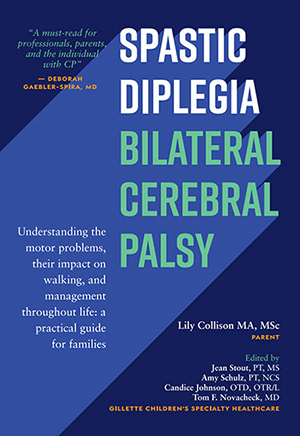
Spastic Diplegia
Bilateral Cerebral Palsy
An empowering and evidence-based guide for living a full life with spastic diplegia–bilateral cerebral palsy
“I highly recommend this book to people who have CP, parents, family members, and medical professionals.”
—Dr. Hank Chambers, Professor of Clinical Orthopedic Surgery, University of California, San Diego, Director of the Southern Family Cerebral Palsy Center at Rady Children’s Hospital, San Diego, Past President, American Academy for Cerebral Palsy and Developmental Medicine, California.